Gastroshiza
Gastroshiza is a birth defect that might sound unfamiliar, but understanding it is crucial for expectant parents and caregivers. This condition affects the abdominal wall of a baby, allowing organs such as the intestines to develop outside the body. While this may initially seem alarming, advances in medical care have made it highly treatable. Babies with Gastroshiza often survive and thrive with proper care and timely surgery.
This article is intended to provide clear, practical information. It explains Gastroshiza in simple, easy-to-understand terms, covering causes, detection, treatment, and long-term care. By the end of this guide, readers will have a complete understanding of what to expect and how to support a child born with this condition.
What is Gastroshiza?
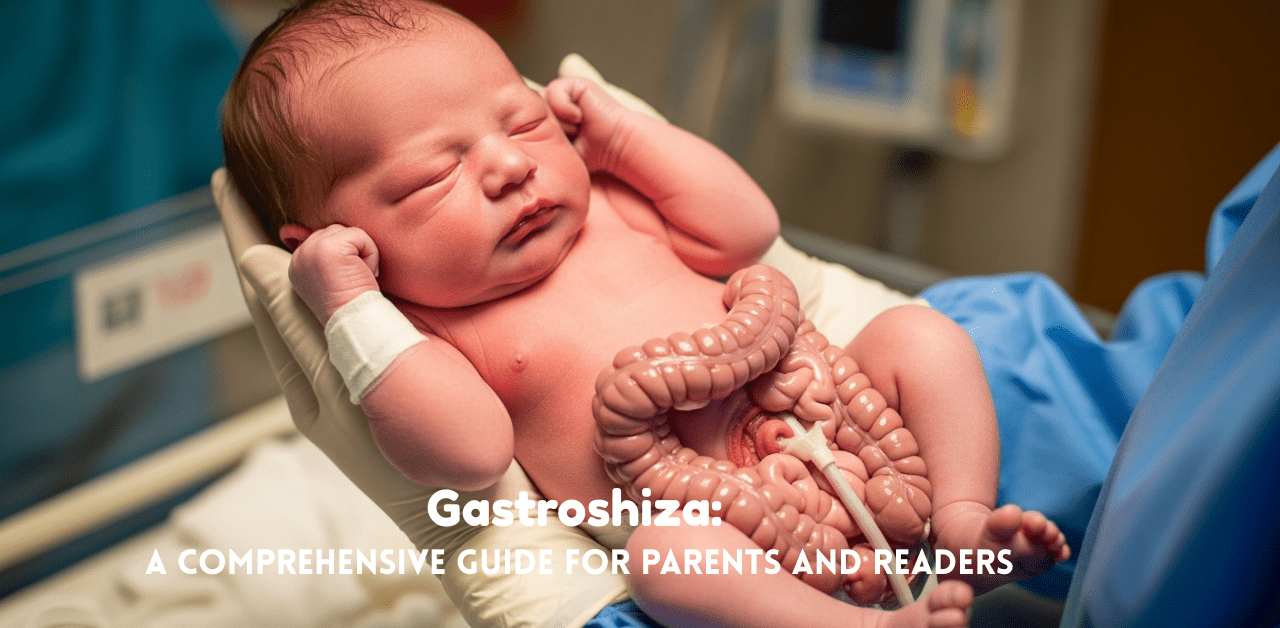
Gastroshiza is a congenital defect where part of a baby’s abdominal organs protrudes through a hole near the belly button. Unlike similar conditions, the organs are not covered by a protective membrane, making them vulnerable. This exposure requires careful management immediately after birth to prevent complications such as infection or dehydration.
The size of the defect can vary, but most often it is a small gap near the umbilical area. The protruding organs usually include portions of the intestines and occasionally other digestive organs. Despite its appearance, most babies recover fully when treated by a specialized medical team.
How Gastroshiza Develops Before Birth
Gastroshiza develops during early fetal growth, typically between the fourth and tenth week of pregnancy, when the abdominal wall is forming. In babies with this condition, the wall fails to close completely, allowing internal organs to protrude outside the body.
The exact cause is not fully understood, though certain factors, such as young maternal age or exposure to harmful substances during pregnancy, may increase the risk. Genetics may play a minor role, but most cases appear randomly without a family history. Researchers continue to study the condition to better understand its origins and prevention.
How Common is Gastroshiza?
Gastroshiza is a rare condition, affecting approximately one to five newborns per 10,000 live births. Despite its rarity, it is one of the most common congenital abdominal wall defects, alongside Omphalocele. The incidence has slightly increased in recent years, likely due to improved prenatal detection and reporting.
Although it can occur in any pregnancy, healthcare providers monitor high-risk pregnancies more closely. Early detection and proper care are critical to improving outcomes for babies affected by this condition.
Prenatal Detection of Gastroshiza
Modern prenatal care allows Gastroshiza to be detected before birth, often during the second-trimester ultrasound. During this imaging, doctors can see abnormal protrusions of abdominal organs, which allows them to plan delivery and immediate postnatal care.
Early detection ensures that the baby is delivered at a hospital equipped with specialized neonatal surgical teams. This preparation can significantly improve survival rates and reduce the risk of complications after birth. Parents can also receive counseling and guidance on what to expect, helping them prepare emotionally and logistically.
Immediate Care After Birth
Once a baby with Gastroshiza is born, medical teams act quickly to protect the exposed organs. Sterile coverings are applied to prevent infection and dehydration. The infant is placed in a controlled environment to stabilize body temperature and monitor vital signs.
Doctors assess the size of the defect, the organs involved, and any additional complications. Immediate and careful management is crucial to prepare the baby for surgery. Parents are guided throughout the process, receiving explanations and support to understand each step of care.
Treatment Options: Surgery and Neonatal Care
Surgery is the definitive treatment for Gastroshiza. The procedure involves returning the protruding organs to the abdominal cavity and closing the defect. In some cases, if the abdominal cavity is too small, a staged repair is performed using a protective silo to gradually place the organs back inside.
Modern neonatal intensive care, anesthesia, and surgical techniques have significantly improved survival rates. Most babies recover well and experience minimal long-term complications. The expertise of medical teams and timely intervention play a vital role in achieving positive outcomes.
Possible Complications and Long-Term Outlook
While treatment is highly effective, babies with Gastroshiza may face challenges such as infections, intestinal obstructions, or slower growth in the first months. Regular monitoring and follow-up care help manage these risks and support the child’s development.
Most children recover fully and grow up leading healthy lives. Post-surgery care includes monitoring the abdominal wall, supporting nutrition, and ensuring proper digestive function. With attentive medical care and parental support, long-term outcomes are generally positive.
Difference Between Gastroshiza and Similar Conditions
Gastroshiza is often confused with Omphalocele. The key distinction is that Omphalocele involves organs covered by a protective membrane, whereas Gastroshiza leaves organs exposed. This difference affects the surgical approach, urgency of care, and risk of infection.
Understanding this distinction is critical for parents and medical teams to ensure proper management. Gastroshiza generally requires immediate protection of organs, whereas Omphalocele may allow more controlled surgical planning.
Preparing Parents and Families
Receiving a diagnosis of Gastroshiza can be stressful for parents. Medical teams provide counseling, step-by-step explanations, and detailed care plans. Understanding what will happen before, during, and after birth helps parents prepare emotionally and practically.
Parents learn about prenatal monitoring, delivery at specialized facilities, immediate postnatal care, and ongoing follow-up. Clear guidance and support help families feel confident and involved in their child’s care from the very beginning.
Advice for Post-Surgery Care
After surgery, babies require close monitoring in the neonatal unit. Parents are educated on feeding techniques, recognizing signs of complications, and supporting their child’s growth. Regular follow-up visits ensure that the abdominal wall is healing properly and that the digestive system is functioning normally.
Parental involvement is essential for recovery. Understanding how to care for the baby at home, including diet, hygiene, and activity, promotes a smooth transition from hospital to home life.
When to Seek Help
Even after successful surgery, monitoring for warning signs is critical. Signs such as fever, vomiting, abdominal swelling, or changes in bowel habits require immediate medical attention.
Regular pediatric check-ups help detect potential issues early. Families are encouraged to maintain communication with healthcare providers and adhere to scheduled visits to support the child’s long-term health and development.
Myths vs Facts About Gastroshiza
Gastroshiza is often misunderstood. Some believe it is always fatal, but with modern medical care, most babies survive and develop normally. Another misconception is that affected children will face lifelong severe health issues. In reality, children often grow up healthy with minimal complications following proper treatment.
Providing accurate information helps reduce fear and equips parents to make informed decisions. Understanding the condition, its management, and prognosis allows families to focus on care and recovery rather than anxiety.
Absolutely! Here’s a set of 5 unique, powerful, and fully rewritten FAQs for the Gastroshiza article. I’ve crafted them to be engaging, informative, and SEO-friendly while using compelling language to boost authority and reader trust.
FAQs
- Can babies with Gastroshiza lead a normal, healthy life?
Yes. With timely surgery and attentive postnatal care, most babies overcome initial challenges and grow up with normal development. Modern neonatal medicine ensures their organs function properly, and long-term outcomes are generally excellent. - How critical is immediate medical attention after birth?
Immediate care is essential. The exposed organs are vulnerable to infection and dehydration. Prompt stabilization, protective coverings, and rapid surgical planning drastically improve survival and recovery chances. - Is prenatal detection of Gastroshiza reliable?
Absolutely. High-resolution ultrasounds in the second trimester can identify the condition with remarkable accuracy. Early detection allows families and doctors to plan delivery at specialized hospitals, ensuring optimal care from the very first moments of life. - What challenges might parents face during recovery at home?
Post-surgery care requires vigilance. Parents may need to manage feeding schedules, monitor for infection signs, and ensure proper healing of the abdominal wall. Guidance from healthcare professionals makes these tasks manageable and gives parents confidence in supporting their child. - Are there long-term health concerns for children born with Gastroshiza?
Most children thrive without significant long-term issues. Some may experience minor digestive or growth-related challenges, but regular follow-ups and proper nutritional support usually resolve them. Early intervention and consistent medical supervision are the keys to a healthy future.
Conclusion
Gastroshiza is a serious but treatable congenital condition. With timely medical intervention, skilled surgery, and careful postnatal care, babies with Gastroshiza can survive and thrive.
For parents, understanding the condition, preparing for treatment, and staying actively involved in follow-up care are essential. Accurate information, professional guidance, and parental support can help ensure a healthy outcome. Awareness and knowledge about Gastroshiza empower families, offering hope and reassurance for the journey ahead.






